Invasive Monitoring: Types, Benefits, Risks, and Applications
"Learn about invasive monitoring techniques used in critical care, including arterial line monitoring, central venous pressure, and ICP monitoring. Discover the benefits, risks, and applications of these procedures."
Invasive monitoring is a critical medical procedure used to collect real-time data from the body, providing healthcare professionals with accurate insights that help manage seriously ill patients. Unlike non-invasive monitoring, invasive monitoring requires the insertion of medical devices into the body. It’s essential in critical care, surgery, and managing complex medical conditions. This article explores what invasive monitoring is, its types, benefits, risks, and applications in medicine.
What is Invasive Monitoring?
Invasive monitoring refers to procedures where medical instruments are inserted into the body to monitor various physiological parameters like blood pressure, heart rate, cardiac output, and intracranial pressure. These measurements are crucial for managing critically ill patients, guiding therapeutic decisions, and monitoring treatment progress.
Why Invasive Monitoring is Used?
Invasive monitoring is often used when non-invasive methods are insufficient, especially for critically ill patients. It allows continuous, real-time monitoring, offering high-accuracy measurements that are vital for making informed decisions in situations where every minute counts.
Types of Invasive Monitoring
Invasive monitoring encompasses various devices and techniques designed to monitor specific physiological parameters. These devices help doctors track a patient's condition in real time.
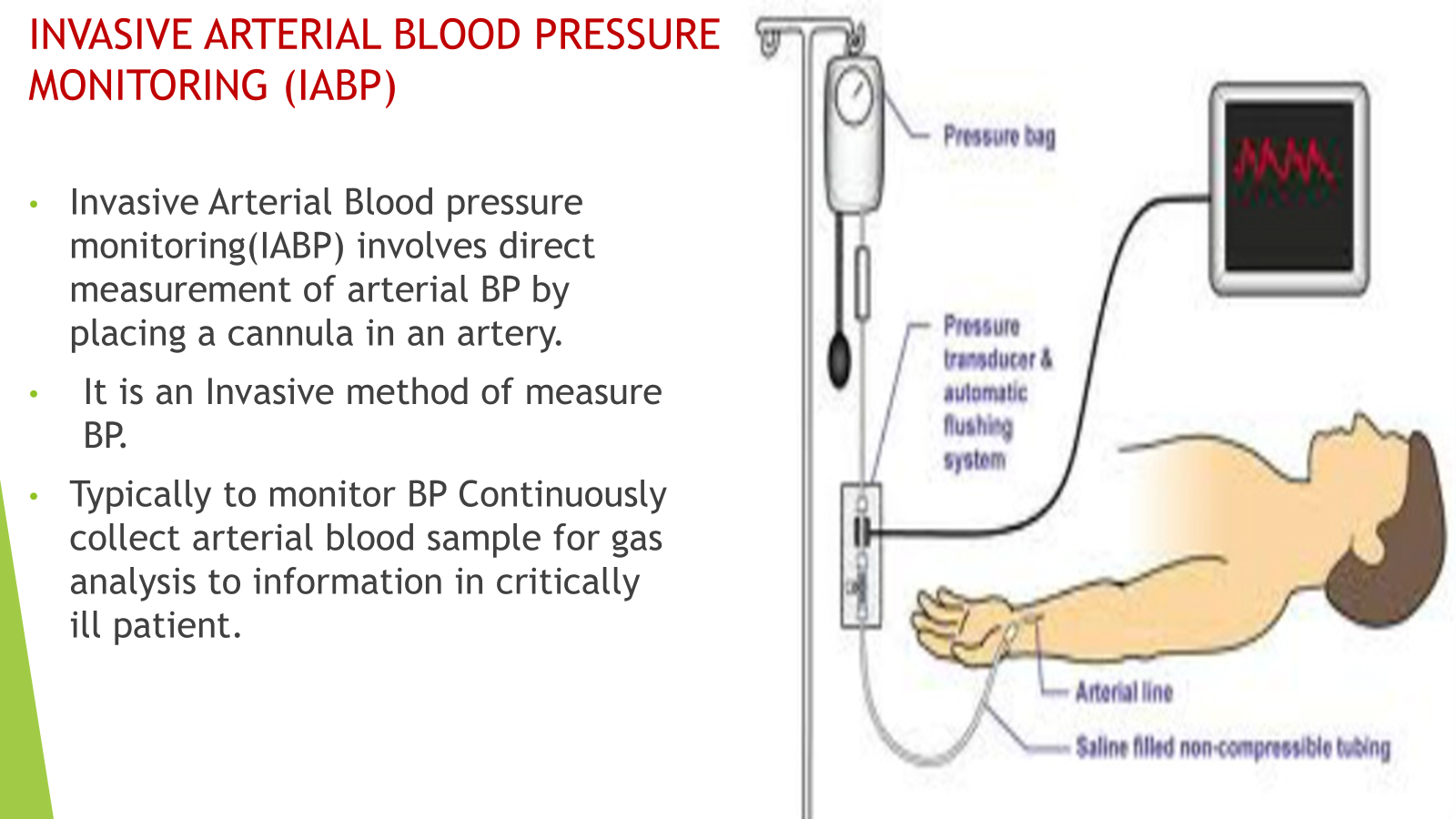
1. Arterial Line (Art-Line) Monitoring
- Procedure: A catheter is inserted into an artery (commonly the radial artery) to provide continuous and accurate blood pressure readings.
- Common Uses: Monitoring blood pressure in critically ill patients, frequent arterial blood gas (ABG) sampling.
- Risks: Infection, bleeding, thrombosis, and arterial damage.
2. Central Venous Pressure (CVP) Monitoring
- Procedure: A catheter is inserted into a large vein (typically the internal jugular or subclavian vein) to measure pressure in the heart’s right atrium, assessing fluid balance and heart function.
- Common Uses: Fluid management, assessing heart function, managing shock and heart failure.
- Risks: Infection, bleeding, pneumothorax, and vessel damage.
3. Pulmonary Artery Catheter (Swan-Ganz Catheter)
- Procedure: A catheter is inserted into a large vein and advanced through the heart to the pulmonary artery, measuring pulmonary artery pressure, cardiac output, and other vital parameters.
- Common Uses: Monitoring cardiac output, assessing pulmonary function, managing sepsis or heart failure.
- Risks: Infection, arrhythmias, rupture of the pulmonary artery, thrombosis.
4. Intracranial Pressure (ICP) Monitoring
- Procedure: A catheter or sensor is inserted into the skull to measure pressure inside the brain, often in patients with traumatic brain injury or hydrocephalus.
- Common Uses: Monitoring for elevated intracranial pressure, managing brain injury, preventing brain herniation.
- Risks: Infection, bleeding, brain tissue damage.
5. Cardiac Output Monitoring
- Procedure: Devices like the Swan-Ganz catheter are used to measure cardiac output, the amount of blood the heart pumps per minute.
- Common Uses: Assessing heart function, managing shock, monitoring fluid balance in critical conditions.
- Risks: Similar to other invasive procedures, risks include infection, bleeding, and mechanical failure.
6. Invasive Blood Gas (ABG) Analysis
- Procedure: Blood is drawn directly from an artery to measure gas concentrations like oxygen, carbon dioxide, and pH.
- Common Uses: Monitoring respiratory function, acid-base balance, metabolic status in critical conditions like respiratory failure or kidney disease.
- Risks: Hematoma, infection, and arterial damage.
Benefits of Invasive Monitoring
Invasive monitoring is highly beneficial in managing critically ill patients by providing continuous, real-time data that helps clinicians make quick, accurate decisions.
1. Real-Time, Continuous Data
Invasive monitoring provides continuous data, which is essential for managing patients with rapidly changing conditions. For example, arterial lines allow for real-time blood pressure monitoring, giving clinicians immediate feedback on treatment adjustments.
2. High Accuracy
Invasive techniques offer more accurate measurements than non-invasive alternatives. For example, central venous pressure provides direct insight into a patient’s fluid status, unlike non-invasive methods, which may not be as reliable.
3. Detailed Insights into Critical Conditions
Invasive monitoring allows for precise evaluation of complex conditions like sepsis, shock, and cardiac failure. Measurements such as pulmonary artery pressure and cardiac output give valuable information to guide treatment.
4. Guiding Therapeutic Decisions
Invasive data is critical for tailoring patient treatment. For example, central venous pressure readings help clinicians decide whether a patient needs additional fluids or vasopressors. In the case of ICP monitoring, real-time pressure data helps prevent brain damage in patients with traumatic brain injury.
Risks of Invasive Monitoring
Despite the many benefits, invasive monitoring comes with several risks. Understanding these risks is crucial for healthcare providers and patients.
1. Infection
The most significant risk of invasive monitoring is infection, particularly in devices like central venous catheters or pulmonary artery catheters. Infections can lead to severe complications, including sepsis or meningitis.
2. Hemorrhage and Thrombosis
There’s a risk of bleeding or clot formation during invasive procedures. For example, arterial lines can cause bleeding or thrombus formation, which can lead to further complications such as embolism or ischemia.
3. Mechanical Failures
Devices used in invasive monitoring, like catheters or sensors, may malfunction, become dislodged, or cause injury to surrounding tissues. Regular monitoring and proper placement are essential to reduce this risk.
4. Organ Damage
The insertion of invasive devices, especially those near vital organs (e.g., heart, brain), carries the risk of damaging organs. For example, a Swan-Ganz catheter can cause rupture of the pulmonary artery, while ICP monitoring can lead to brain damage if not performed correctly.
Applications of Invasive Monitoring
1. Critical Care
Invasive monitoring is extensively used in ICUs to manage patients with shock, sepsis, heart failure, and respiratory distress. Continuous data allows for precise management of fluids, medications, and other treatments.
2. Cardiac Surgery
Invasive monitoring is essential during heart surgeries to track cardiac output, blood pressure, and oxygenation in real-time. It helps guide anesthetic management and ensures patient stability during complex procedures.
3. Trauma and Neurological Emergencies
For patients with brain injuries or conditions that may cause increased intracranial pressure, ICP monitoring is vital. It provides critical data for preventing brain herniation and optimizing brain perfusion.
4. Respiratory Failure
Invasive monitoring of cardiac output, pulmonary artery pressure, and oxygen saturation helps guide the treatment of patients with respiratory failure or ARDS (acute respiratory distress syndrome). This data helps in adjusting mechanical ventilation and oxygen therapy.
Alternatives to Invasive Monitoring
While invasive monitoring provides detailed, continuous data, non-invasive methods are often used for routine monitoring in stable patients. Some common non-invasive alternatives include:
Pulse oximetry for oxygen saturation
Blood pressure cuffs for periodic blood pressure readings
Electrocardiograms (ECG) for heart rhythms
Non-invasive cardiac output monitors like bioimpedance devices